Lung Cancer
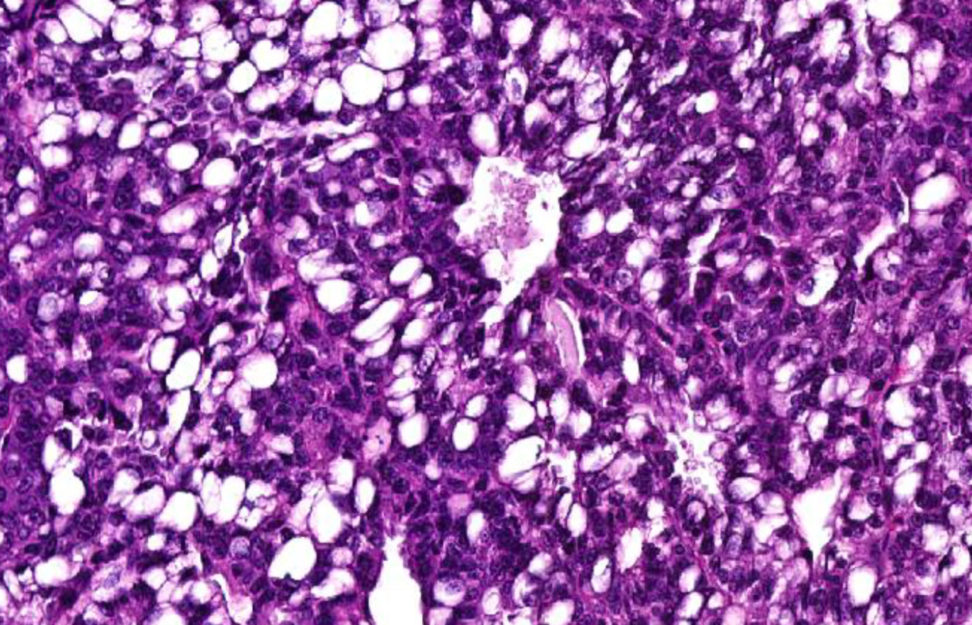
There are two main types of lung cancer that are classified by the type of cell affected. Non-small cell lung cancer – this occurs in 85% of cases and small cell lung cancer.
Anyone can get lung cancer. Smoking, occupational exposure, pollution and genetics are key risk factors that increase a person’s chances of getting it. However, it is often diagnosed at late stages because symptoms can be vague, sometimes there are no symptoms and the cancer is found during routine tests.
At Centenary our research into this deadly cancer is looking at the impact of inflammation and potential treatments around a number of areas. These include whole genome sequencing, molecular impacts of infections, oxidative stress on the lungs and the role of our diet and microbiome.
Our research
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
Inflammation is a critical driver of many disease features of lung cancer. There are many different processes that contribute to inflammation including inflammatory epithelial cells, macrophages, mast cells, complement system and inflammasomes, that we have high level expertise in. We have specific tools that we can use to define their specific roles and which are most important in driving lung cancer.
Oxidative stress and immunometabolism, the study of metabolic pathway usage in an immune cell, are major drivers in cancer and other chronic respiratory diseases. We have several new compounds, some naturally derived, that target and suppress these factors at their source. This source is damaged mitochondria that become dysfunctional when exposed to cigarette and bushfire smoke, air pollution and other environmental challenges.
We are analysing the microbial populations (the microbiome) and the factors that they produce (metabolites) in the lung and the gut. The research looks at how the microbiome drives or protects against lung cancer.
We are also looking at how these results can be modified with specific dietary components.
Finding mutations that are biomarkers of the early development of lung cancer in easy accessible samples. We have found a range of mutations in the lungs in advanced lung cancer in mice and are working backwards to see when they first emerge and predict the development of lung cancer. We are confirming these mutations in blood and airway cells.
Epigenetics is the study of processes that modify DNA without affecting its sequence. We are working out how epigenetics change in the lung, in particular we look at microRNA, acetylation and methylation. We also look at how these change the activity of diseases and drive disease features.
This is the study of processes that modify DNA without affecting its sequence. We are working out how these change in the lung (microRNA, acetylation, methylation) and how they change the activity of diseases and drive disease features.
We are performing several studies where we perform high throughput analysis of different groups of factors (mRNA, microRNA, proteins, phosphoproteins, lipids, microbiomes, metabolomes, acetylation, methylation). We can integrate all of these analyses together to obtain a more holistic view of how cancer develops and progresses, and we can also identify pivotal factors that control different parts of the disease and may be more effective targets.
We can use our expertise in each of these areas to develop new therapies to prevent or reverse the development of disease features in cancer and other related diseases such as asthma, pulmonary fibrosis, COVID-19 and COPD.
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
Our research
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
Inflammation is a critical driver of many disease features of lung cancer. There are many different processes that contribute to inflammation including inflammatory epithelial cells, macrophages, mast cells, complement system and inflammasomes, that we have high level expertise in. We have specific tools that we can use to define their specific roles and which are most important in driving lung cancer.
Oxidative stress and immunometabolism, the study of metabolic pathway usage in an immune cell, are major drivers in cancer and other chronic respiratory diseases. We have several new compounds, some naturally derived, that target and suppress these factors at their source. This source is damaged mitochondria that become dysfunctional when exposed to cigarette and bushfire smoke, air pollution and other environmental challenges.
We are analysing the microbial populations (the microbiome) and the factors that they produce (metabolites) in the lung and the gut. The research looks at how the microbiome drives or protects against lung cancer.
We are also looking at how these results can be modified with specific dietary components.
Finding mutations that are biomarkers of the early development of lung cancer in easy accessible samples. We have found a range of mutations in the lungs in advanced lung cancer in mice and are working backwards to see when they first emerge and predict the development of lung cancer. We are confirming these mutations in blood and airway cells.
Epigenetics is the study of processes that modify DNA without affecting its sequence. We are working out how epigenetics change in the lung, in particular we look at microRNA, acetylation and methylation. We also look at how these change the activity of diseases and drive disease features.
This is the study of processes that modify DNA without affecting its sequence. We are working out how these change in the lung (microRNA, acetylation, methylation) and how they change the activity of diseases and drive disease features.
We are performing several studies where we perform high throughput analysis of different groups of factors (mRNA, microRNA, proteins, phosphoproteins, lipids, microbiomes, metabolomes, acetylation, methylation). We can integrate all of these analyses together to obtain a more holistic view of how cancer develops and progresses, and we can also identify pivotal factors that control different parts of the disease and may be more effective targets.
We can use our expertise in each of these areas to develop new therapies to prevent or reverse the development of disease features in cancer and other related diseases such as asthma, pulmonary fibrosis, COVID-19 and COPD.
Professor Phil Hansbro, Director of the Centenary UTS Centre for Inflammation leads this research.
